
As the name suggests it is a condition in which there is a long term inflammation of the pancreas. The pancreas is a digestive organ located in the upper part of your tummy, below your liver and behind the stomach. It produces the digestive enzymes needed for digestion of food and the hormones including Insulin needed to control the blood sugar levels.
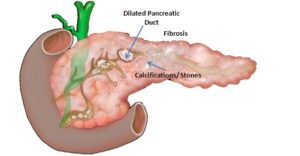
Chronic pancreatitis develops slowly over time and leads to irreversible damage to the pancreatic tissue. The pancreas gets so much damaged, that it becomes hard and shrunken. During this process, the duct of the pancreas becomes narrow and strictured at one or multiple places. Especially near its opening in the intestine, ultimately leading to stone formation in the pancreatic duct. This leads to the failure of normal emptying of the pancreatic digestive juices in the intestine after a meal. Eventually, the whole duct dilates and is filled with stones.
The inflammation is triggered by alcohol intake and smoking in predisposed patients. Other reasons for this chronic inflammation of the pancreas are genetic factors, autoimmune conditions, nutritional factors. In a certain group of patients, the cause of pancreatitis remains unknown.
The hallmark symptom of chronic pancreatitis is abdominal pain. Pain is chronic and intermittent initially, which over time becomes more frequent or even constant. It is severe stabbing in nature, localized to the upper part of your tummy between your navel and chest. The pain may radiate to the back and is often triggered by eating, especially high fat foods. Pain after eating occurs as the digestive juice secreted by the pancreas to digest the meal gets entrapped inside the pancreas causing increased pressure in the duct.
With time the pain becomes more severe and debilitating. In some cases, it may become constant. Constant pain occurs due to the entrapment of the nerves in the hard and inflamed pancreas. Some of these patients take painkiller tablets every day and may need repeated injections as well to control their pain. For many patients, this pain is so debilitating that they are not able to lead a normal life.
When the pancreas doesn’t work properly, it affects the body’s ability to digest the food properly. Hence some patients of chronic pancreatitis do not get the required nutrients from the food they eat. This leads to the problem of malnutrition, leading to weak bones and vision loss. Patients may struggle to gain or maintain their weight.
Oily foul smelling bowel movements and weight loss may be seen in the advanced stages of chronic pancreatitis. It indicates that the pancreatic tissue that is actively functional for your digestion is very less.
Patients may also develop diabetes due to the loss of pancreatic tissue and may need insulin to maintain a good blood sugar control.
Some patients of chronic pancreatitis develop jaundice. The lower part of the bile duct goes through the pancreas. And sometimes as the pancreas becomes hard and shrunken, it compresses the bile duct. This leads to the blockage of the bile flow from the liver to the intestine and causes jaundice. 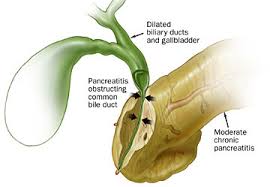
Another complication of chronic pancreatitis is pseudocyst formation. Due to persistent blockage and increased pressure in the pancreatic duct, there is a leakage of pancreatic juice from the duct. Leading to damage to the surrounding area and the formation of an infected cystic-like structure. 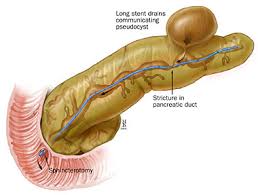
In some patients, there is clot formation in the portal vein. The Portal vein is located just behind the pancreas and in some patients, pancreatitis may cause direct damage to this vein. Portal vein thrombosis may lead to splenomegaly and vomiting of blood.
Blood tests are usually not helpful in the diagnosis of chronic pancreatitis. Serum Amylase is normal in most patients, except if there is a superadded episode of acute pancreatitis.
A CT scan will show that the pancreas is shrunken and the pancreatic duct is dilated. It also shows that stones are formed within the tube. Some patients may have stone formation even outside of the duct in the pancreatic tissue or the side branches of the duct.
Information about the other complications of chronic pancreatitis like, leakage of duct and pseudocyst formation, blood clot formation in portal vein and enlargement of spleen are also obtained from a CT scan. As these complications may change the treatment plan, knowing about them is very important.
MRCP is a specialized MRI done to see the details of the dilated pancreatic duct, stones in the duct and the side branches of the duct. It also gives information about the bile duct, weather it is dilated or not. Details that we get in an MRCP are very very important in the planning of treatment in chronic pancreatitis.
The primary goal of treatment is to achieve long-term pain relief, maintain nutrition, to slow down the further progression of the disease, control of the complications associated with the disease, and to restore the quality of life. Triggers like alcohol, smoking, and certain drugs should be avoided to prevent further damage to the pancreas.
Good pain management is a very important part of treatment. This includes oral painkillers like NSAIDs, narcotic medications, injectable medications and interventional procedures like celiac nerve blocks.
Pancreatic enzyme supplement and avoidance of high fat food are also measures to control pain. These measures are also important from the nutritional point of view.
In cases, when there are pancreatic duct stones and narrowing, the stones need to be removed and drainage of pancreatic juice should be established. Removal of the stones and relieving the block and establishing a good flow of the pancreatic juice in the intestine does slow down further damage to the pancreas. This helps in preventing further complications and the development of advanced chronic pancreatitis. It can be achieved by an endoscopic procedure called ERCP or by a formal surgery.
 In this procedure, an endoscope is passed through your mouth to the part of the intestine where the duct of the pancreas opens. Then a guidewire is passed from this opening into the duct. Once a guidewire is in place, a dilator is passed over this wire to dilate the duct at the site of narrowing or structure. Stones are removed with the help of a balloon catheter.
In this procedure, an endoscope is passed through your mouth to the part of the intestine where the duct of the pancreas opens. Then a guidewire is passed from this opening into the duct. Once a guidewire is in place, a dilator is passed over this wire to dilate the duct at the site of narrowing or structure. Stones are removed with the help of a balloon catheter.
Many a time ESWL, that is external shock ware therapy is used before doing this endoscopic treatment, to break the stone (similar to the ones done for kidney stones). It the end, a stent is placed in the duct, which needs to the exchanged repeatedly as necessary for about 1 year.
In a selected group of patients with less load of stones and smaller stones and less number of narrowing or blockage, this should be the first line of treatment. The patients who respond well to this procedure can be saved from surgery.
ERCP is now a standard procedure and gives good results in many patients. But we should keep in mind that even if it is a minimally invasive treatment option, it still does have its own risk. Especially when it is needed to be repeated multiple times.
Surgery is the last resort for patients who are troubled in spite of maximum medical management and endoscopic treatment.
All those patients who had undergone an ERCP and stenting, but are still having episodes of pain even after 6-8 weeks of stenting should consider surgery for better relief of pain and improvement in the quality of life.
Those patients who had undergone multiple endoscopic stenting and still need more stent exchanges should also consider surgery as a more preferred and an onetime solution to their problems.
Patients who have advanced chronic pancreatitis, having complications like jaundice, portal vein thrombosis or pseudocyst are the right candidates for surgery.
The type of surgery varies depending on the severity of the problem and the associated complications.
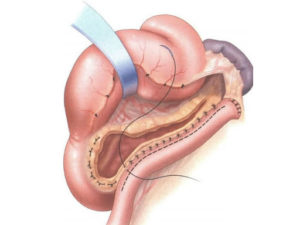
For most of the patients, the surgery includes the opening of the whole duct of the pancreas, removal of all the stones, removal of a small portion of the pancreas from the head of the pancreas and attaching the whole duct to the intestine. This surgery is called Frey’s procedure.
The history of the evolution of this surgery gives us the understanding that doing anything less than this does not give complete long term relief of pain. For example, if the tail part of the duct is not opened or the tissue from the head part is not removed, or if the stones from the side branches of the duct are not removed then the results are inferior. This is because in such a case some part of the pancreas is not drained, and the digestive juice from this part still remains trapped, and cause inflammation and pain.
And this is the exact reason why with ERCP multiple procedures and stent exchanges are needed. Because the drainage to the juices is provided by a 10 f stent which is just the size of refill of our pen. While in surgery the whole duct is opened to intestine creating a very wide opening. This new opening is not likely to be blocked again and further formation of stone is unlikely if the surgery is done in a proper way.
Although surgery is a major undertaking when done after thorough evaluation and in a proper manner, the risks are minimal and give excellent long term results. Pain free life, good nutritional status and good quality of life.
For deciding the treatment option, the success rate should be weighed carefully against the number of procedures required to accomplish and maintain this success rate and the risk of complications associated with these procedures.
According to Cochrane study which compiles all the studies does throughout the world, Endoscopic drainage seems inferior to surgery in symptomatic patients with advanced Chronic Pancreatitis.
You should consult a specialist to figure out what is the best treatment plan for you. The specialist will decide your treatment depending on your age, the severity of your pain, whether you have developed diabetes or exocrine enzyme deficiency and other complications of chronic pancreatitis. With timely and proper treatment, a patient of chronic pancreatitis can lead a normal and pain free life.
Listen to a few of our patients who fought the battle against chronic pancreatitis by clicking the below link
Hope this information was helpful to you in some ways. Any further queries or concerns you can call us or send you reports to us on 8156078064 or mail us on drchiragthakkar1307@gmail.com